Investigation HDC6446 – Informed Consent Fraud Cover Up
http://www.hdc.org.nz/decisions/search-decisions/1999/97hdc6446/
This is where it all began. The HDC established a protection mandate to surgeons, which effectively defrauded cholecystectomy patients of their rights, and at the same time covered up breaches of the Code. Here we see:
- The HDC somehow, strangely fails to identify breaches of patient rights, including the right to be advised of treatment risks.
- The surgeon was then given a free pass.
- Yet, the HDC acknowledges a shortfall in surgical practices – A breach of the Code for not providing informed consent, or an explanation and disclosure of risks. By admission, the HDC confirmed a breach of the Code took place, yet gave a free pass.
- Then, the HDC reviewed and signed-off misleading ‘fake’ informed consent documentation on cholecystectomy surgery, which was absent of major risks, side effects affecting quality of life and void of alternative non-surgical treatment options. As a result, the documentation cannot be used to legally obtain informed consent.
- The HDC becomes an accessory to New Zealand’s largest medical fraud.
The HDC Mandate to defraud health consumers – established protection tabled
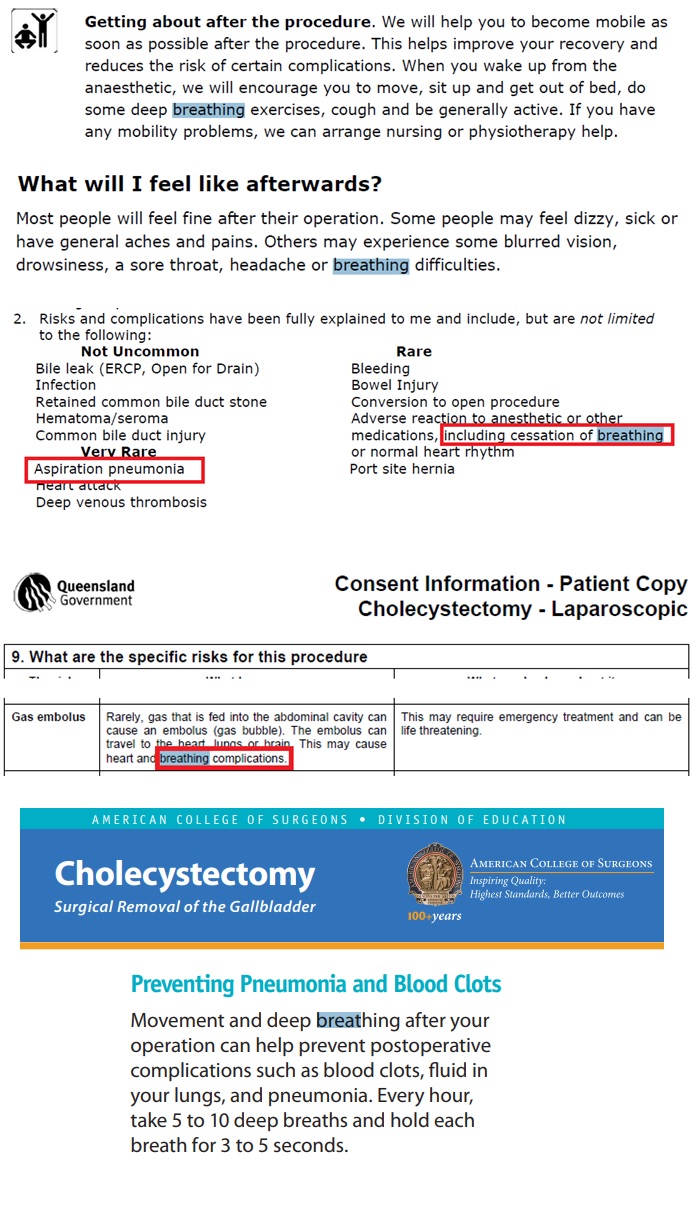
The HDC reviewed and signed New Zealand surgeon’s gold standard patient information brochure about laparoscopic gallbladder surgery. Nowhere in the Royal Australasian College of Surgeons (RACS) Brochure of Laparoscopic Gallbladder Surgery is the word ‘death’ mentioned as a risk. Nor is there ANY alternative treatment options or side effects affecting quality of life considered. This can be considered a lack of critical information and paramount to obtaining informed consent through deception.
In reality, the information brochure breaches patients’ rights by omitting very relevant information that a reasonable consumer, in that consumer’s circumstances, would require to make an informed choice, or give informed consent. The information brochure makes statements which are easily proved as false, in order to obtain informed consent. The documentation confirms this by strongly advising patients that it is their responsibility to seek a discussion with a second surgeon in order to obtain information surrounding the risks of surgery.
This laparoscopic surgeons ‘get out of jail’ out-clause detailed: “The aim of this pamphlet (Informed consent patent information hand out) is to provide you with general information”, “and does not contain all the known facts about gallbladder surgery or every possible risk and benefit.”
Yet the HDC reviewed and signed off that it meets patients’ rights to make an informed consent.
Because of this, the HDC can be directly held accountable for blocking patients’ rights to make an informed consent decision. As a result, they are an accessory to the fact, in obtaining consent fraudulently through the means of deception and are also accountable for any resulting harm.
The HDC “I support the surgeon’s intention to provide patients with a copy of the newly published Royal Australasian College of Surgeons’ Patient Handout for Laparoscopic Cholecystectomy. In my opinion, it is likely that if the consumer had had access to this detailed information some of her (informed consent) concerns (about risks) may have been more swiftly alleviated.”
This document used to obtain informed consent, in effect, breaches patient’s Right 6(1), (2) and Right 7(1) of the Code of Health and Disability Services Consumers’ Rights.
Click here for more evidence – FAKE, misleading informed consent forms
Take Home Points
- The HDC ruling effectively provided a protection mandate for cholecystectomy surgeons, allowing New Zealand’s largest on-going health consumer surgical fraud to originate (based on numbers).
- Every informed consent for laparoscopic cholecystectomy in New Zealand is obtained illegally by deception. Obtaining consent illegally is a criminal offence and it is obtained through coercion, deception and concealment, a misrepresentation of risks, side effects affecting quality of life and alternative non-surgical treatment options. This deception occurs under the direct protection of the HDC and is in breach of the Code of Health and Disability Services Consumers’ Rights (the Code).
- New Zealand cholecystectomy surgeons are given a free pass under the HDC’s perceived application of the legally enforceable Code of Rights. Effectively the HDC are promoting and encouraging a policy of ‘learning not lynching’ towards medical practitioners and protecting them.
Code of Rights breaches the HDC somehow, strangely fail to investigate or identify:
|
Right to make an informed choice and give informed consent Right 6(1)(b) Every patient have the right to the information that a reasonable consumer in his circumstances would expect to receive, including an explanation of the alternative treatment options available and an assessment of the expected risks, side effects (affecting quality of life), benefits and costs of each option. Failing to disclose risks during the informed consent process breached Right 6(1) (b) of the Code of Health and Disability Services Consumers’ Rights (the Code). Right 7(1) Every patient right to make an informed choice and give informed consent Every consumer has the right to make an informed choice and give informed consent. Services may be provided to a consumer only if that consumer makes an informed choice and gives informed consent. Without this information, patients are denied that opportunity to legally give informed consent. |
|
Failure to Disclose Harm Doctors have a care duty to provide patients full disclosure when something goes wrong during an operation, (disclose harm or injury). Right (1) (a) of the Code provides that patients have the right to be treated with respect. Failure to disclose inadvertent harm involves tacit deception – respect for patient autonomy supports a truthful and sensitive discussion about what went wrong and why. Right 6(1) of the Code affirms every consumer’s right to the information that a reasonable consumer, in that consumer’s circumstances, would expect to receive. When a surgical complication occurs, the patient is entitled to open, truthful, and timely information about the complication, its effect and its significance Right 5(2) of the Code every patient has the right to an environment that enables both patient and doctor to communicate openly, honestly, and effectively. Open and honest communication requires candour about inadvertent harm on the part of the doctor; |
What Happened
A patient complained, in layman’s terms that during the course of surgery, the provider, a surgeon, ‘cut her muscle and liver causing significant blood loss’. In addition, the patient complained that ‘she sustained a collapsed lung following the surgery’.
The HDC Outcome
The HDC concluded that no treatment injury occurred, as the patient described it. Instead, it was a result of the patient’s imagination and it was concluded that no breach of the code took place either.
However the HDC did go on to recommend that surgeons should provide patients with ‘informed consent documentation’ detailing surgery risks, in order meet informed consent requirements. The HDC decided in this case that her informed consent was apparently NOT met.
The HDC: ‘In my opinion, it is likely that if the consumer had had access to this detailed information (disclosed treatment risks) some of her concerns may have been more swiftly alleviated.’
Breaches of patient rights not investigated (unanswered questions)
But In reality, there was no evidence presented showing that informed consent had been provided, displaying the procedural risks. The patient made a complaint and the surgeon also failed to disclose the true nature of post-surgical issues and injury, to both the patient, and the HDC.
This brings us to the point, why do surgeons lie?
|
Why Laparoscopic Cholecystectomy Surgeons lie? Why would a reasonable surgeon lie to patients about alternative gallstone treatment options, expected risks and side effect risks affecting quality of life (Right 6 of the Code), in order to obtain consent for Cholecystectomies and/or even consider performing unneeded surgical procedures? From a surgeon’s perspective there are three distinct answers:
Philip F. StahelEmail author, Todd F. VanderHeiden and Fernando J. Kim. Why do surgeons continue to perform unnecessary surgery? https://doi.org/10.1186/s13037-016-0117-6
Quote from Royal Australasian College of Surgeons spokesman Dr John Quinn said it was “almost certain” the medical industry influenced surgical decisions. “But we cannot control what individual surgeons do in any given situation. It’s up to them to diagnose and treat their patients as they see fit.” And why would a surgeon provide an inaccurate and incomplete testimony to the HDC or to ACC treatment injury clinical reviews? One explanation can be found in the Medical Council of New Zealand Good Medical Practice guide that sets the standard for cultural competence, clinical competence and ethical conduct for doctors. It states: “You must cooperate fully with any formal inquiry or inquest into the treatment of a patient (although you have the right NOT to give evidence that may lead to criminal proceedings being taken against you)”. In other words a Doctor does NOT have to be forth coming with any information that would incriminate and lead to criminal proceedings |
The Evidence in More Detail:
Who is telling the truth, the surgeon or the patient?
In the HDC’s own words, The surgeon had professional obligations to both the consumer, and the hospital he was operating in, to advise the consumer of the injury sustained.’
Injury 1:
Patient not advised when injury sustained – Injury resulting bleeding and blood loss
“During the surgery the surgeon noticed that an artery within a muscle was bleeding and he extended the incision in order to suture the artery and thereby stop the bleeding”
Note: Bleeding complications account for up to one third of all major complications seen in laparoscopic cholecystectomy, and are the second most common cause of death in patients undergoing the procedure (after anaesthesia-related complications)[2].
- This amounts to a breach of the Code: The repair to the blood vessel injury should have been advised to the patient from the start of the post-operation follow up.
Injury 2:
Patient not advised when injury sustained – Possible collapse lung more than likely
- The HDC: “The investigation found that the consumer did not suffer a collapsed lung following the surgery. Further to this, the investigation found no evidence that any lack of reasonable care and skill on the part of the surgeon contributed to the breathing difficulties experienced by the consumer after the surgery”
- The HDC: “A chest x-ray was taken and this revealed some minor failure of the lung to expand, a condition known as atelectasis, which is common in patients who undergo upper abdominal surgery. This is different from a collapsed lung where the lung partially deflates due to injury”.
More About: Atelectasis (at-uh-LEK-tuh-sis) — a complete or partial collapse of a lung or lobe of a lung — develops when the tiny air sacs (alveoli) within the lung become deflated. It’s a breathing (respiratory) complication after surgery [3]
The risk of pulmonary complications is as high as 8%: The incidence of pulmonary complications after upper abdominal or chest surgery (incl. cholecystectomy) are known to be associated with marked declines in lung volume and a high risk of postoperative pulmonary complications. Laparoscopic cholecystectomy, (8%) showed abnormal spirometry data. 30 to 39% of patients with abnormal spirometry showed less severe PPC such as atelectasis, lung collapse and pleural effusion. Less severe PPC disappeared within second to third postoperative days [4]
Source reference: ‘Breathing exercises are likely to have a beneficial effect on respiratory muscle strength in patients undergoing upper abdominal surgery (cholecystectomy) Surgery’ [5]
Summary of breaches again not identified by the HDC:
- Breach of the Code, Right 6(1) (b) – Failed to disclose risks to patient, thus the complaint made.
- Breach of the Code, Right 1(a) – Failed to disclose harm when injury occurred.
- Breach of the Code, Right 4(1) – Failure to provide adequate post-care support in a manner that minimised the potential harm, such as post-surgery breathing exercises.
Unanswered Questions Continued:
Question 1: Did a breach of common law take place with consent not legally obtained? Does this extend to a criminal offence and did the HDC cover up consent fraud?
In order for consent to be legally obtained, the following requirements need to be met under a legally enforceable Code of Health and Disability Services Consumers’ Rights (the Code): An absence of such information would indicate fraud:
| Did the health service provider / surgeon:
1] Advise of alternate treatment options 2] Advise of post treatment side effect risks affecting quality of life And as such, 3] Did the consumer receive reasonable information in order to make an informed choice? And did the HDC conceal these breaches in his investigation |
Answer
NO NO S NO YES |
Question 2: Did the HDC invoke their ‘not lynching policy’, in order to overlook the health consumer’s complaint and provide a free pass to the surgeon for breaches of the Code?
The HDC: “ A chest x-ray was taken and this revealed some minor failure of the lung to expand, a condition known as atelectasis, which is common in patients who undergo upper abdominal surgery. This is different from a collapsed lung where the lung partially deflates due to injury”
Reviewing previous information on atelectasis risks, ‘a complete or partial collapse of a lung or lobe of a lung’, amounts to an injury not disclosed or admitted to the patient. This is in fact is an obvious breach of the Code.
References:
- Disclosure of harm – Medical Council of New Zealand. https://www.mcnz.org.nz/assets/News-and-Publications/Statements/Disclosure-of-harm.pdf
- Kaushik, R. (2010). Bleeding complications in laparoscopic cholecystectomy: Incidence, mechanisms, prevention and management. Journal of Minimal Access Surgery, 6(3), 59–65. http://doi.org/10.4103/0972-9941.68579
- Atelectasis – Symptoms and causes – Mayo Clinic https://www.mayoclinic.org/diseases-conditions/atelectasis/symptoms-causes/syc-20369684
- Sha M, Kohno M, Yamagami J, Fujiwara Y, Hiroshima N, Kitahara M, Yamauchi K, Ohmura A. Pulmonary complications following laparoscopic cholecystectomy in patients with abnormal spirometry. https://www.ncbi.nlm.nih.gov/pubmed/11797360
- Samantha T. Grams, Lariane M. Ono, Marcos A. Noronha, Camila I. S. Schivinski, Elaine Paulin. Breathing exercises in upper abdominal surgery: a systematic review and meta-analysis. http://www.scielo.br/pdf/rbfis/v16n5/aop049_12_sci1056.pdf
- Altomare DF, Rotelli MT, Palasciano N. Diet after cholecystectomy. https://doi.org/10.2174/0929867324666170518100053
- Wikipedia, Postcholecystectomy syndrome. https://en.wikipedia.org/wiki/Postcholecystectomy_syndrome
- Murshid KR. The postcholecystectomy syndrome: A review. Saudi J Gastroenterol [serial online] 1996 [cited 2018 Jan 15];2:124-37. Available from: http://www.saudijgastro.com/text.asp?1996/2/3/124/34017