FAKE, Illegal Informed Consent Patient Hand Out – Royal Australasian College of Surgeons (RACS) Brochure of Laparoscopic Gallbladder Surgery
A doctor is under a duty of care to take reasonable steps to ensure that all patients are aware of any material risks involved in any recommended treatment. Doctors are also under a duty of care to advise of reasonable alternatives or variant treatments. The test of materiality is whether, in the circumstances of the particular case, a reasonable person, in the patient’s position, would be likely to attach significance to the risk, or whether the doctor is, or should be reasonably aware that the particular patient would be likely to attach significance to the risk.
Excepting to this ethical principle – a New Zealand laparoscopic cholecystectomy surgeon operating under protection.
The documentation below is used by New Zealand laparoscopic cholecystectomy surgeons, at District Health Boards, to obtain illegally required informed consent for treating patients’ gallstones and gallbladder issues.
The true intention of the current informed consent documentation for laparoscopic cholecystectomy surgery is to obtain consent by deception and misrepresentation with a deliberately crafted concealment of all side effect risks and alternative non-surgical treatment options. There is a preference to withhold treatment options so that patients’ feel that surgery is their only choice, which equals financial gain for surgeons. This is fraud by false representation and is also a criminal offence under the Crimes Act 1961 No 43 (as at 28 September 2017), Public Act 240
This documentation can be used in a court of law as evidence: New Zealand laparoscopic cholecystectomy surgeons (under the direct protection of the HDC) are committing the following unlawful criminal offences on patients under the Crimes Act 1961:
- Negligence causing injury,
- Assault and battery for touching a person without the patient providing full consent;
- Obtaining consent dishonestly through coercion and misuse of position of trust.
This behavior is deception, misrepresentation and coercion. It is a deliberate concealment of risks, side effects and alternative non-surgical treatment options. As such, it is a breach of the legally enforceable Code of Health and Disability Services Consumers’ Rights (the Code).
As employers, District Health Board are liable under Section 72(2) of the Health and Disability Commissioner Act 1994 for failing to prevent the acts, or omissions, of employees. They are vicariously liable for criminal negligence causing harm and injury. Including conspiring to block services that would lead to the diagnosis and treatment for known post surgery side effect complications. As such, they are exposed as having complicit involvement in this fraud.
Trivialising the nature of the harm and downplaying the risks in order to obtain consent by a laparoscopic surgeon is a serious issue. Morally and ethically, it can be likened to the behaviour of narcissistic sociopaths. Those involved are displaying the integrity of serious criminals who are intentionally causing harm, with terrifying outcomes. Violating patients’ rights without hesitation is not just greedy, but also evil. (LWNGB)
Step 1: Lie about the occurrence of gallstones and explain to the patient they are part of a small minority unlucky to have them causing pain
Misconception presented:
“About one adult in every 10 has gallstones”
Truth:
Gallstones are common; they occur in approximately 20% of women in the US, Canada and Europe. 20% of people over 60 have a single large stone, or as many as several thousand smaller ones.
Step 2: Lie about the importance of the gallbladder’s function and what it actually does
Misconception presented:
“The gallbladder (simply just) stores bile”
Truth:
The gallbladder does not simply just store bile, but also stores and concentrates bile, during the fasting state (between meals). Bile is concentrated five-fold in the gall bladder by absorption of water and small electrolytes which increases its potency and intensifies its effect on fats. The gallbladder also largely contributes to the regulation of bile composition by unique absorptive and secretory capacities.
“Cholecystectomy(removing the gallbladder) increases the enterohepatic recirculation rates (circulation of biliary acids from liver to digestive tract back to liver) of bile acids leading to metabolic effects and an increased risk of nonalcoholic fatty liver disease, cirrhosis, and small-intestine carcinoid, independently of cholelithiasis”
Housset C1, 2, Chrétien Y1, 2, Debray D1, 3, Chignard N1. Functions of the Gallbladder. https://doi.org/10.1002/cphy.c150050
Misconception presented:
“Bile aids digestion by breaking down fat”
Truth:
Your gallbladder is part of the digestive system. The gallbladder is triggered to release concentrated bile during a meal. Bile also neutralises excess stomach acid after it leaves the stomach and before it enters the duodenum, the first section of the small intestine. The digestion enzymes in the small intestine work best in alkaline environment.
Step 3: Lie about the lack of Doctors understanding and awareness of why gallstones come into being
Misconception presented:
“Doctors do not know exactly why some people get gallstones and others don’t”
Truth: about what cause gallstones is never disclosed to patients by New Zealand surgeons when conducting a diagnosis and alternative treatment options:
Most of this information is never disclosed to clients, intentionally blocking patients from receiving sufficient relevant information to make an informed decision about alternative treatment options.
There are three types of gallstones [20] (i) Pure cholesterol stones, which contain at least 90% cholesterol, (ii) pigment stones either brown or black, which contain at least 90% bilirubin and (iii) mixed composition stones, which contain varying proportions of cholesterol, bilirubin and other substances such as calcium carbonate, calcium phosphate and calcium palmitate. Causes are due to:
Age
- Gallstones are 4-10 times more frequent in older than younger subjects
- About a quarter of women over 60 years will develop them [13]
Gender:
- Women during their fertile years are almost twice as likely as men
- Increased levels of the hormone oestrogen, as a result of pregnancy or hormone therapy, or the use of combined (oestrogen-containing) forms of hormonal contraception, may increase cholesterol levels in bile and also decrease gallbladder movement, resulting in gallstone formation [60]
Diabetics
- People with diabetes generally have high levels of fatty acids called triglycerides. These fatty acids may increase the risk of gallstones.
- Gallbladder function is impaired in the presence of diabetic neuropathy, and regulation of hyperglycaemia with insulin seems to raise the lithogenic index [24]
Genetics
- Cholesterol gallstone prevalence varies widely, from extremely low (<5%) in Asian and African populations, to intermediate (10-30%) in European and Northern American populations, and to extremely high (30-70%) in populations of Native American ancestry (Pima Indians in Arizona, Mapuche Indians in Chile) [53]
Obesity and body fat distribution
Rapid weight loss
- Rapid weight loss is associated with occurrence of sludge and gallstones in 10-25% of patients in a few weeks of initiating the slimming procedures [61]
Post pregnancy
Diet
- Nutritional exposure to western diet, i.e., increase intake of fat, refined carbohydrates and decrease in fibre content is a potent risk factor for development of gallstones [65,66]
- The biliary calcium concentration plays a part in bilirubin precipitation and gallstone calcification [40,41] Many patients with gallstones have increased biliary calcium, with supersaturation of calcium carbonate [42]
- Calcium intake seems to be inversely associated with gallstone prevalence [67] Dietary calcium decreases cholesterol saturation of gallbladder bile by preventing the reabsorption of secondary bile acids in the colon.
- Vitamin C influences 7α hydroxylase activity in the bile and it was shown that ascorbic acid might reduce lithogenic risk in adults. [68]
- Coffee consumption seems to be inversely correlated with gallstone prevalence, due to an increased enterohepatic circulation of bile acids. Coffee components stimulate cholecystokinin release, [69] enhance gallbladder motility, inhibit gallbladder fluid absorption, decrease cholesterol crystallization in bile [70] and perhaps increase intestinal motility. [71,72]
Physical activity (lack of)
- Sedentary behaviour is positively associated with the risk of cholecystectomy. [17]
Drugs (PPI’s, Opioids, Contraception)
- The lithogenic role of ceftriaxone [36,37] can also precipitate in the gallbladder as sludge [38]
- Use of the somatostatin analogue octreotide, has been cited as another contributing factor in the development of gallstones. [43]
- All fibric acid derivatives increase biliary cholesterol saturation while lowering serum cholesterol.
- Clofibrate is a potent inhibitor of hepatic acyl-CoA cholesterol acyltransferase (ACAT).
- ACAT inhibition leads to an increased availability of free or unesterified cholesterol for secretion into bile, favouring gallstone formation. [24]
- Prolonged use of proton pump inhibitors has been shown to decrease gallbladder function, potentially leading to gallstone formation. [73]
- Oestrogen treatment also reduces the synthesis of bile acid in women
Other
- Cholesterol supersaturation for in obese persons
- Defective conversion of cholesterol to bile acids in the non-obese
- Interruption of the enterohepatic circulation of bile acids during overnight fasting
- Fasting in the short term increases the cholesterol saturation of gallbladder bile and in the longer term, causes gallbladder stasis which can lead to sludge, and eventually gallstone formation. Younger women with gallstones were shown to be more prone to skip breakfast than controls. [63] A shorter overnight fasting is protective against gallstones in both sexes. [64]
- Pigment stones occur when red blood cells are being destroyed, leading to excessive bilirubin in the bile.
- Black pigment stones are more common in patients with cirrhosis or chronic hemolytic conditions such as the thalassemias, hereditary spherocytosis, and sickle cell disease, in which bilirubin excretion is increased. [28,29]
- Primary bile-duct stones are associated with infection
- Primary brown pigment stones of the bile ducts often occur in Asians, associated with decreased biliary ecretory Immunogloblin A (IgA.)[30]
- Prolonged total parenteral nutrition, [35] starvation, or rapid weight loss. [36,37]
- Impaired motility of the gallbladder as seen in patient with high spinal cord injury [43]
Njeze, G. E. (2013). Gallstones. Nigerian Journal of Surgery : Official Publication of the Nigerian Surgical Research Society, 19(2), 49–55. http://doi.org/10.4103/1117-6806.119236
Step 4: Refuse to investigate what the root causes of pain could really be and if the gallbladder has really failed
Misconception presented:
“The decision to have treatment is made after discussion with your surgeon. If gallstones are present and are thought to be causing trouble, you surgeon will recommend the best treatment for you”
He we see the trap is set, only the surgeon will investigate and decide on treatment. This definitive response is demonstrably false, misleading and deceptive. The ‘good’ surgeon will make this statement to justify a lack of alternative treatment options to their patients, because there is no known root causes to address and treat. Resultantly, for the patient, there is no option but to undergo surgery, or do nothing. The trap is set and the patient feels compelled to have surgery.
Truth:
| Right 6(2) Every patient has the right to an explanation of their condition, and with sufficient information to enable them to make an informed choice |
Misconception presented:
“If you are uncertain about the advice you have received, you may wish to seek a second opinion form another surgeon”
Here the patient is directed only to another surgeon for their opinion. There is no option for the patient to discuss their situation with a Gastroenterologist (i.e possibly offering assessment for dissolution treatment) or a holistic Naturopathic doctor (i.e possibly offering treatment assessment to normalise bile composition leaving the liver, dissolve existing gallstones in the gallbladder, prevent the reabsorption of bile and cholesterol in the small intestine) , who have been known to openly criticise and disagree with New Zealand surgeons’ willingness to operate only.
New Zealand surgeons instead advise patients using an in-house system and surgery is presented as a one-stop treatment and patients are led to believe that no concerning or real side effects or alternative treatment option do not exist. As a result the likelihood of receiving an honest disclosure, is slim to none.
With holding this information or denying even the existence of alternatives is a breach of the code, informed consent is obtained illegally, by fraudulent deception
| Right 7(1) Every consumer has the right to make an informed choice and give informed consent. Services may be provided to a consumer only if that consumer makes an informed choice and gives informed consent. Without this information, patients are denied the opportunity to legally give informed consent. |
The behaviour from surgeons has the result of guaranteeing future clients, as patients will be reluctant to do nothing. It is a ‘my way or the highway’ approach adopted by surgeons. No alternative treatments are offered, such as diet change or medications. This is a breach of the Code.
Truth:
“First of all, I believe it is nearly criminal what traditional medicine is doing to our public when it comes to managing this problem. It is RARELY ever indicated to remove someone’s gallbladder. If one ignores warning symptoms and does not address the reasons why their gallbladder is not functioning properly, than the disease can progress to the point where the pancreas is inflamed or the gallbladder is seriously infected and may have to be removed to save a person’s life.
So, not only are surgeons removing these organs unnecessarily, but in their nutritional ignorance they are telling patients that their gallbladders do not serve any purpose and they can live perfectly well without them. This is a lie. The gallbladder serves an important digestive function”
Dr. Mercola, Licensed physician and surgeon.
Failure to properly investigate, right to services of an appropriate standard
Doctors and surgeons are required investigate a patient’s condition. Failure to correctly diagnose, carry out tests, or accurately assess any health problems in order to provide the right course of treatment is grounds for medical malpractice. Quite simply, confirming the presence of a gallstone through ultrasound does NOT provide clear diagnosis for the removal of patients’ gallbladders.
Failure to appropriately investigate conditions is breach of the Code of Rights
| Right 4(1) Every consumer has the right to have services provided with reasonable care and skill.
Right 4(4) Every consumer has the right to have services provided in a manner that minimises the potential harm to, and optimises the quality of life of, that consumer |
Misconception presented:
“After you have had a thorough examination, your surgeon can discuss the diagnosis with you. If gallstones are present and are thought to be causing trouble, the surgeon will recommend the best treatment for you”
Surgeons are currently leading patients towards the option of surgery and presenting surgery as the only course of action. A thorough investigation, tests into cause of gallstones is almost never done. ie Decreased gallbladder function due to taking medications such as is never explored such as “Opioid Induced Hypo-functional Gallbladder disease”
Truth:
| Right 4 (2) Every consumer has the right to have services provided complying with legal, professional, ethical and other relevant standards. |
“Gallstones are sometimes implicated as the source of symptoms in patients with dyspepsia. However, such an association should be made cautiously, since gallstones may silently coexist in patients with dyspepsia, and other causes of dyspepsia are more common.”
Dr David Maplesden, Medical Advisor, Health and Disability Commissioner
“A significant number continue to experience symptoms (PCS) and thus patients should be thoroughly assessed and evaluated preoperatively. Furthermore, the presence of dyspepsia in a patient with gallstones does not automatically imply that the gallstones are the cause. Patients should be advised of both the risks of surgery and the risk of postoperative persistence of symptoms.”
S.S.JaunooS.MohandasL.M.Almond. Postcholecystectomy syndrome (PCS) [ScienceDirect]
“The existing knowledge on risk factors for negative symptomatic outcome should be integrated in clinical decision making, with regard to guidelines for the indication of cholecystectomy and consideration of alternative treatment options” … “As cholecystectomy is not beneficial to all patients, distinguishing patients with a heightened risk of persisting and emerging symptoms at 6 weeks (post surgery) is important”
Literature mentions pre-operative dyspeptic symptoms, pre-operative flatulence, and experiencing over three symptoms of flatulent dyspepsia as predictors of negative post-cholecystectomy outcomes, such as post-cholecystectomy syndrome and persistence of a bothersome symptom”
C. Mertens & J. De Vries & V. P. W. Scholtes & P. Jansen & J. A. Roukema Prospective 6 Weeks Follow-up Post-cholecystectomy: The Predictive Value of Pre-Operative Symptoms. https://link.springer.com/content/pdf/10.1007/s11605-008-0718-1.pdf
Investigation tests can include:
- Ultrasonography,
- Trans abdominal ultrasonography,
- Endoscopic ultrasonography (EUS),
- Cholescintigraphy (HIDA scan),
- Endoscopic retrograde cholangio-pancreatography (ERCP)
Step 5: Refuse to provide alternative treatment options and do nothing
Misconception presented:
“There is no known treatment or diet that can prevent gallstones”
“Although symptoms due to gallstones may go away, they tend to come back if the condition is left untreated. Such patients are more likely to develop complications “
These statements are outright lies. Laparoscopic cholecystectomy surgeons’ have full knowledge of the alternative options surrounding the treatment of gallstones. Also, they have a conflicting, vested financial interest in deceiving patients.
Truth:
| Right 6 – Every patient has the right to be fully informed, to receive an explanation of the options available and be provided with sufficient information to enable patients to make an informed choice. |
Extracts from other consent forms confirms this lie:
Queensland Government health Services: Cholecystectomy – Laparoscopic informed consent document
“Alternative treatments: Oral Dissolution Therapy. Oral dissolution therapy is the taking of chemicals by mouth to dissolve the gallstones. It is most effective for patients who are not overweight, in a younger age group, have small or single gall stones and a gall bladder that is working well”
Cholecystectomy Laparoscopic consent form
(See Appendices – About truths undisclosed and the treatment for gallstones being one of surgeons’ bread and butter revenue earner)
Note: District Health Board are advising very commonly that patients wait 6 -18 months before requiring treatment, or assessment by other specialists. Surgeons who are doing nothing and offering no alternative non-surgical treatment options, during this period, can be considered to be guaranteeing a further client for surgery. This omission of action is a failure to provide a duty of care to the patient. This is a breach of Right 4(4), ‘Every consumer has the right to have services provided in a manner that minimises the potential harm to, and optimises the quality of life of the consumer.’ Alternative treatment options should include diet changes and bile salt dissolution.
Doing nothing, also known as “watchful waiting” is the simple act of letting patients become sick and is part of the surgeons’ business model. Surgeons provide limited advice and the “wait and see” method of diagnosing and treating patients is meant to keep them sick, guaranteeing further business cash flow for surgeons, through surgery. The existence of this policy is backed by previous HDC investigation rulings and is known medical ethics. HDCXXXX, HDCXXXX
The truth about alternative treatment options never disclosed:
Submission 1: Ursodeoxycholic acid
Dissolution of Gallstones: ursodeoxycholic acid, Actigal®, is a medicine that can be given as a pill to dissolve gallstones. Therapy requires at least 6 to 12 months and is successful in dissolving stones in 40-80% of cases. When surgery is too risky, the symptoms are mild, the stones are small, and rich in cholesterol, dissolution of gallstones is a reasonable alternative.
American College of Gastroenterology http://patients.gi.org/topics/gallstones-in-women/
Submission 2: Percutaneous cholecystostomy:
(PC), a technique that consists of percutaneous catheter placement in the gallbladder lumen under imaging guidance, has become an alternative to surgical cholecystostomy in recent years. Indications of PC include calculous or acalculous cholecystitis, cholangitis, biliary obstruction and opacification of biliary ducts. It also provides a potential route for stone dissolution therapy and stone extraction. Response rates to PC in the literature are between the range of 56-100% as the variation of different patient population. (First performed by an American surgeon, Dr. John Stough Bobbs, in 1867)
Akhan O1, Akinci D, Ozmen MN. Percutaneous cholecystostomy. https://www.ncbi.nlm.nih.gov/pubmed/12204405
Submission 3: Contact dissolution of cholesterol gallstones with organic solvents
The availability of safe, effective cholesterol solvents and solvent transfer devices means that cholesterol gallbladder stones can be eliminated rapidly and safely by CDOS, without the risk of general anesthesia or surgical dissection of the gallbladder bed. Patients with single gallstones are better candidates for CDOS than are patients with multiple gallstones because recurrence after dissolution is less common. Contact dissolution may well be judged the treatment of choice by the medical-surgical gallstone management team in some patients.
Hofmann AF1, Schteingart CD, vanSonnenberg E, Esch O, Zakko SF. Contact dissolution of cholesterol gallstones with organic solvents. https://www.ncbi.nlm.nih.gov/pubmed/2022421
Submission 4: Extracorporeal shock-wave lithotripsy:
Extracorporeal shock-wave lithotripsy (ESWL) is an infrequently used method for treating gallstones, particularly those lodged in bile ducts. ESWL generators produce shock waves outside of the body that are then focused on the gallstone. The shock waves shatter the gallstone, and the resulting pieces of the gallstone either drain into the intestine on their own or are extracted endoscopically. Shock waves also can be used to break up gallstones via special catheters passed through an endoscope at the time of ERCP.
Jay W. Marks, MD. Gallstones. https://www.medicinenet.com/gallstones/article.htm
Submission 5: Bile acid dissolution therapy:
Medical therapy with oral bile acids is appropriate for patients who present with small cholesterol stones and for patients with larger cholesterol gallstones who cannot or will not have surgery. Oral bile acids may also be valuable in the treatment of gallstone recurrence before it has become symptomatic or to prevent recurrence after prior success Am J Surg. 1989 Sep; 158(3): 198-204.
Hofmann AF. Medical dissolution of gallstones by oral bile acid therapy. The American Journal of Surgery. https://doi.org/10.1016/0002-9610(89)90252-3
Submission 6: Watchful waiting help treat gallstones:
Though a gallstone episode can be extremely painful or frightening, almost a third to half of all people who experience an attack never have a recurrence. In some cases, the stone dissolves or becomes dislodged. Because the problem may solve itself without intervention, many doctors take a wait-and-see approach following the initial episode.
Step 6: Refuse to disclose any side effect risks that would affect patients’ quality of life
Misconception presented:
“It is not unusual for a surgeon to dwell at length on every possible side effect”….” However, it is important that you have enough information to weigh up the benefits, risks and limitations of the surgery ”
This consent form actually acknowledges that the actions of New Zealand surgeons are in beach of code of rights when using this information to obtain ‘legal’ consent for treatment
Note: There is no mention of what the side effects are. This is an omission and intent to mislead, breaching patients’ legally enforceable rights and the central principles of ethical behaviour to respect the rights, autonomy and freedom of choice of the patient without exploitation.
From a surgeon’s perspective, creating chronic side effects is more preferable than curing patients of root causes because it is bad for business! The same can be said for advising patients of these side effects.
But according to New Zealand surgeons, the only side effect risk worth dwelling on is to disclose that some people (who over indulge in fatty foods) may develop “diarrhoea”. No other side effect risks are disclosed whatsoever.
Truth:
Every patient has the right to be fully informed
| Right 6(2), Right to be fully informed and to receive an explanation of expected side effects (risks) |
Misconception presented:
“In a few people, too many fatty foods may contribute to loose bowel movements and stomach discomfort. In such cases, a low-fat diet may be helpful.”
“You may have some gas pains and other discomfort while your digestive system returns to normal. During this period, eat healthy food that was easy to digest before your gallbladder surgery.”
“Most people who have their gallbladder removed can return to a normal diet following recovery. Avoid fatty foods at first and slowly add them to the diet, as you prefer.”
“Once your gallbladder has been removed, bile will still flow (as it always has) from the liver to the small intestine.”
There is a continued misconception that after surgery everything will return to normal.
Truth:
There is no evidence-based medical study known to mankind backing these claims presented to patients in order to obtain consent. These definitive claims are nothing more than dishonest, delusional revenue based fantasies. At the very least it is fraudulent, deceitful behaviour by omitting the true risks and lying to patients. Furthermore, sending a patient home without support needed to mitigate or manage the onset of well-documented post surgery problems is an intent to commit grievous body harm and can cause serious health complications that can be both chronic and life long.
The truth about Postcholecystectomy side effects is never disclosed to patients, in order to illegally obtain consent by deception:
The Postcholecystectomy Syndrome (PCS) is a heterogeneous group of diseases and symptoms presenting following gallbladder removal. Symptoms occur in about 5 to 40 per cent of patients who undergo cholecystectomy, and can be transient, persistent or lifelong. The chronic condition is diagnosed in approximately 10% of postcholecystectomy cases.
Post-cholecystectomy Syndrome may include:
- Diarrhoeaas a troublesome problem range from 9 to 12% of which bile acid malabsorption (BAM), 65% of these patients. [1]
- Depression disordersoccurring in 0.9%-3.0% of patients [2]
- Bile (duodenogastric) refluxoccurring in 20%-30% of patients [3,4,5]. Likely damage attributable to chronic bile exposure post-cholecystectomy includes:
-
- Cellular damage to esophagogastric junction
- Bile induced Gastroesophageal Mucosal Injury (Protective barrier that constrains the acidic reflux)
- Increase the incidence of gastric and esophageal cancer
- Sphincter of Oddi dysfunction (SOD) is seen in 1% of patients after cholecystectomy, but in 14%-23% of patients with the post-cholecystectomy syndrome [6]
- Increased Body Mass Index (weight gain) with metabolic syndrome, gastritis, liposoluble vitamin deficiency. Cholecystectomy can have nutritional and metabolic consequences and in the long-term[7]
The onset of symptoms may range from 2 days to 25 years. There may also be gender-specific risk factors for developing symptoms after cholecystectomy. In one study, the incidence of recurrent symptoms among female patients was 43%, compared to 28% of male patients.”
Patients with cholecystectomy had more comorbidities, particularly chronic fatigue syndrome, fibromyalgia, depression, and anxiety. Postcholecystectomy gastroparesis patients had increased health care utilization and had a worse quality of life.
“The absence of the gallbladder leads to functional biliary hypertension and increased hepatic and common bile duct. 3-5 years after cholecystectomy increases right and left hepatic ducts equity.
Functional hypertension in the common bile duct contributes to the appearance of functional and hypertension in Wirsung’s pancreatic duct with the development of the phenomena of chronic pancreatitis . At the same time period in some patients this is accompanied by the progression of chronic pancreatitis, sphincter of Oddi dysfunction and duodenogastric (Biliary / bile ) reflux.
Duodenogastric reflux of mixture of bile with pancreatic juice promotes atrophic gastritis in the antral part of stomach.
From 40% to 60% of patients after cholecystectomy dyspeptic suffering from various disorders, from 20% to 40% of pains of different localization .
Up to 70% of patients after cholecystectomy have chronic effects of “bland” cholestasis, chronic cholestatic hepatitis and chronic compensatory bile acid-dependent apoptosis of hepatocytes.
Patients undergoing cholecystectomy had an increased prevalence of metabolic risk factors for cardiovascular disease, including type 2 diabetes mellitus, high blood pressure, and high cholesterol levels.
Part of patients after cholecystectomy with increased concentration of hydrophobic hepatotoxic co-carcinogenic deoxicholic bile acid in serum and/or feces with increased risk of colon cancer”
Biliary Diseases Laparoscopic Cholecystectomy. Postcholecystectomy Syndrome Dr. Jacob L. Turumin (Iakov L. Tyuryumin), MD, PhD, DMSci
“The incidence of postcholecystectomy syndrome has been reported to be as high as 40% in one study, and the onset of symptoms may range from 2 days to 25 years. There may also be gender-specific risk factors for developing symptoms after cholecystectomy. In one study, the incidence of recurrent symptoms among female patients was 43%, compared to 28% of male patients.”
“cholecystectomy is associated with several physiological changes in the upper gastrointestinal tract which may account for the persistence of symptoms or the development of new symptoms after gallbladder removal. The cholecyst sphincter of Oddi reflex, cholecyst-antral reflex, and cholecyst-oesophagal reflexes are all disrupted and some local upper gastrointestinal hormonal changes also occur after cholecystectomy. Thus, there is an increased incidence of gastritis, alkaline duodene gastric reflux and gastro-oesophageal reflux after cholecystectomy, all of which may be the basis for postcholecystectomy symptoms.”
Postcholecystectomy syndrome (PCS), S. Mohandas, L.M. Almond, Department of General Surgery, Worcestershire Royal Hospital, Worcester, UK
“Instance of Post Cholecystectomy Syndrome sustainably increased when patients followed for 5-9 years vs. only two years’ follow-up”
The postcholecystectomy syndrome: A review, Khalid R Murshid, Department of Surgery, King Khalid University Hospital, Riyadh, Saudi Arabia
“Patients with cholecystectomy had more comorbidities, particularly chronic fatigue syndrome, fibromyalgia, depression, and anxiety. Postcholecystectomy gastroparesis patients had increased health care utilization and had a worse quality of life.”
Cholecystectomy and Clinical Presentations of Gastroparesis, the NIDDK Gastroparesis Clinical Research Consortium (GpCRC)*
“The basic role of the gallbladder in a human is a protective. The gallbladder decreases the formation of the secondary hydrophobic toxic bile acids (deoxycholic and lithocholic acids) by accumulating the primary bile acids (cholic and chenodeoxycholate acids) in the gallbladder, thus reducing their concentration in gallbladder-independent enterohepatic circulation and protecting the liver, the mucosa of the stomach, the gallbladder, and the colon from their effect”
Jacob L. Turumin, Victor A. Shanturov, Helena E. Turumina Irkutsk Institute of Surgery, Irkutsk Regional Hospital, Irkutsk 664079, Russia
The truth about the claims of the
“digestive system returns to normal, return to a normal diet”
Guideline for medical nutrition therapy (MNT) post-cholecystectomy:
“MNT should be individualized based on the patient’s issues and a number of diet modifications may be indicated. Fat intake should be limited for several months to allow the liver to compensate for the gallbladder’s absence, should be introduced gradually, and excessive amounts at any one meal should be avoided. Increased fiber intake will help normalize bowel movements. Be sure to increase the amount of fiber slowly over several weeks. It has been suggested that adding soluble fiber to the diet will act as a sequestering agent and bind the bile in the stomach between meals to avoid gastritis. If reflux is an issue, avoid alcohol, caffeinated and carbonated drinks, chocolate, citrus foods and juices, coffee, vinegar-based dressing, onions, tomato-based foods, spicy foods, and mint, and eat smaller meals.”
What Medical Nutrition Therapy Guideline Is Recommended Post-Cholecystectomy? Marcason, Wendy
Journal of the Academy of Nutrition and Dietetics, Volume 114, Issue 7, 1136 https://www.ncbi.nlm.nih.gov/pubmed/24956996
Diet After Cholecystectomy:
“Cholecystectomy can have nutritional and metabolic consequences in the short-term (diarrhea, abdominal pain and bloating) and in the long-term (increased Body Mass Index with metabolic syndrome, gastritis, liposoluble vitamin deficiency). Pathogenic mechanisms behind these disturbances are reviewed and the need for an early post-operative nutritional intervention based on low-lipid, high-fibers diet, is highlighted.”
Donato F. Altomare*, Maria T. Rotelli, Nicola Palasciano. Diet After Cholecystectomy . Current Medicinal Chemistry Volume 24, 201 http://www.eurekaselect.com/node/152535/article
“People without a gallbladder are more prone to digestive problems and liver problems; they can even form stones within the ducts of the liver. The risk of developing a fatty liver is also greater in people without a gallbladder”
“Your liver continues to manufacture bile, but there is no longer a place to store it or concentrate it. Therefore bile continually slowly trickles into intestines. If you eat a fatty meal, you will not be able to secrete a large enough amount of bile into your intestines, therefore the fat will be poorly digested. This means many people experience diarrhea, bloating, nausea or indigestion. Not digesting fat well means you will not be able to digest essential fatty acids, including omega 3 and omega 6 fats. It also means you’ll have a hard time absorbing fat soluble vitamins such as vitamins D, E, A and K. These nutrients are vital for good health, and you will probably need to take a supplement.”
What to do if you don’t have a gallbladder. Dr Sandra Cabot M.D
“In 5 – 40% cholecystectomies new symptoms have appeared, symptoms which affect the life quality of the patients who underwent the surgical operation.”
“The proper diet can be a solution, and it is advisable to limit the food that can aggravate diarrhea, foods with a high content of fat, fried foods and sauces. Elevating the fiber quantity helps in normalizing the intestinal transit. Small and more frequent meals ensure a better combination of the alimentary chime with the available bile. An adequate diet after cholecystectomy should include small amounts of weak proteins, such as lacteous products, fish or chicken, non-fat meat, accompanied by vegetables, fruit and cereals. We have recommended this diet for patients with cholecystectomy. We obtained good results, none of these patients have not required hospitalization for symptoms framed in PCS syndrome”
Diet and Postcholecystectomy Syndrome (PCS) Daniela Radu, Doina Georgescu, M. Teodorescu Journal of Agroalimentary Processes and Technologies. http://journal-of-agroalimentary.ro
Truth about the claim that bile flow returns to normal:
The following is withheld from patients in order for them to remain unaware of the high risk of digestion issues:
- The gallbladder stores and concentrates bile between meals.
- The gallbladder also largely contributes to the regulation of bile composition by unique absorptive and secretory capacities
- Cholecystectomy increases the enterohepatic recirculation rates of bile acids leading to metabolic effects and an increased risk of nonalcoholic fatty liver disease, cirrhosis (a condition in which the liver does not function properly due to long-term damage.), and small-intestine carcinoid, independently of cholelithiasis.
Housset C1,2, Chrétien Y1,2, Debray D1,3, Chignard N1. Functions of the gallbladder. https://doi.org/10.1002/cphy.c150050
“In general, (Postcholecystectomy Syndrome )PCS is a preliminary diagnosis and should be renamed with respect to the disease identified by an adequate workup. It arises from alterations in bile flow due to loss of the reservoir function of the gallbladder. Two types of problems may arise. The first is continuously increased bile flow into the upper gastrointestinal (GI) tract, which may contribute to esophagitis and gastritis. The second is related to the lower GI tract, where diarrhea and colicky lower abdominal pain may result.”
Steen W Jensen, MD; Chief Editor: John Geibel, MD, DSc, MSc, AGAF Postcholecystectomy Syndrome [medscape.com]
More about Postcholecystectomy Syndrome (PCS) symptoms:
http://lifewithnogallbladder.com/faq/postcholecystectomy-syndrome-pcs/
Step 7: Misrepresent, minimise and conceal the actual risks so as to never tell the truth:
Misconception presented:
“An injury to a bile duct can cause leakage or obstruction of the duct. A return to theatre and more surgery may be needed to repair the problem”
This statement about one of the more serious risks is a complete misrepresentation and fails to provide an adequate explanation of the true extent of the risk that a patient would expect from a surgeon.
Truth:
Code of Ethics of the New Zealand Medical Association: “If it can be shown that a doctor has failed to provide adequate information and thereby failed to ensure that the patient comprehends, so far as is possible, the factors required to make decisions about medical procedures, such failure could be considered medical misconduct and could be the subject of disciplinary proceedings.”
The right of patients to be fully informed:
| Right 6(2) Every patient has the right to an explanation of risks affecting their quality of life, as well as sufficient information to enable them to make an informed choice. |
“The incidence of Bile Duct Injury (BDI) during laparoscopic cholecystectomy has decreased but remains as high as 1.4%” “Despite the excellent functional outcome after repair, the occurrence of a BDI has a great impact on the patient’s physical and mental quality of life, even at long-term follow-up”
Boerma, D., Rauws, E. A. J., Keulemans, Y. C. A., Bergman, J. J. G. H. M., Obertop, H., Huibregtse, K., & Gouma, D. J. (2001). Impaired Quality of Life 5 Years After Bile Duct Injury During Laparoscopic Cholecystectomy: A Prospective Analysis. Annals of Surgery, 234(6), 750–757. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1422134/
Truth:
“Conversion from a laparoscopic cholecystectomy to open surgery is not a complication of procedure but rather is done to protect the patient”
This statement is actually truthful. A conversion to open cholecystectomy required when the patient is bleeding to death would be described as a complication if it wasn’t listed as an anticipated complication for laparoscopic cholecystectomy.
From a doctor’s medical definition, a complication is an unexpected event. The following are also not unexpected event ‘complications’:
- Visceral injury
- Duodenal perforation 02
- Colon perforation 02
- Intraoperative hemorrhage
- From cystic artery 04
- From gallbladder bed 21
- From hepatic artery 02
- Bile duct injuries
- Right hepatic duct lesions 02
- Common bile duct partial lesions 06
- Common bile duct total section 04
- Bile leakage from the gallbladder bed 02
Genc, V., Sulaimanov, M., Cipe, G., Basceken, S. I., Erverdi, N., Gurel, M., … Hazinedaroglu, S. M. (2011). What necessitates the conversion to open cholecystectomy? A retrospective analysis of 5164 consecutive laparoscopic operations. Clinics, 66(3), 417–420. http://doi.org/10.1590/S1807-59322011000300009
However, despite this statement being true, there is no mention of recovery details that can take 4-8 weeks, or the fact that open gallbladder surgery side effects can include the following symptoms:
- Pain in your belly. You may also have pain in one or both shoulders for several days after surgery. This comes from the gas still in your belly after your surgery.
- Incision pain for 1 to 2 weeks.
- Sore throat from the breathing tube. Sucking on ice chips or gargling may be soothing.
- Nausea, and maybe throwing up (vomiting).
- Loose stools after eating. This may last 4 to 8 weeks.
Step 8: In order to confirm consent, provide information presented in the patient information form and make any of the following claims without advising of alternative treatment options or truth about side effect risks
- A gallbladder that forms a stone is, by definition, diseased and the only safe treatment to remove a diseased gallbladder is by a ‘cholecystectomy’
- There are no successful alternatives to removing / treating gallstones apart from a ‘cholecystectomy’
- ‘You don’t need a gallbladder’. ‘So surgery to take it out is often recommended’
- ‘You can lead a perfectly normal life without a gallbladder’.
- ‘Your liver will still make enough bile to digest your food but, instead of being stored in the gallbladder, it drips continuously into your digestive system’
- ‘Surgery side effects are temporary. (Bloating, flatulence and diarrhoea – this can last a few weeks)’
- Eat a normal diet straight away – you can return to a normal diet
- Only some people experience symptoms similar to those caused by gallstones after surgery (tummy pain, indigestion, diarrhoea).
- In most cases symptoms are mild and short-lived
- Very rarely, patients notice that their bowels are a little looser (diarrhoea) than before the operation.
- You will be able to eat a normal diet after your operation
- Unfortunately there is no non-surgical alternative; the only successful treatment is to remove (the gall bladder and) gallstones completely.
- Can I manage without my gallbladder? Yes. The gallbladder is a reservoir for bile and we are able to manage without it.
- Very rarely, patients notice that their bowels are a little looser (diarrhoea) than before the operation.
- You will be able to eat a normal diet after your operation
- “Generally once the gallbladder is removed the symptoms you have had will resolve. In some instances they may persist for a short time and then get better”
- “Removal of the gallbladder does not usually impair the digestive system”
- “There are no other effective, safe, durable and widely accepted alternatives to surgery”. “The other alternative is to have no treatment.”
- “You may experience some diarrhoea after surgery. This should settle within three or four weeks. If the diarrhoea is bothersome your local chemist can advise you on over-the-counter remedies.”
- “Your gallbladder is not an essential organ. If it is removed, bile flows to your intestines directly from your liver and digestion continues as normal.”
Step 9: Obtain patient’s signature for consent illegally
Following the presentation of patient information, by the surgeon or in this case the GP , and considered to be truthful and honest, the patient is then asked to sign a consent form acknowledging having been provide consent when in fact :
- Lied to and received no advice or offered any alternative treatment options
- Lied to and misrepresented (provided false statements) about expected risks and outcomes
- Lied to about side effects (affecting quality of life) both chronic and long term
- In breach of the following legally enforceable Code of Rights, the Code of Health and Disability Services Consumers’ Rights (the Code).
| Right (1)(a) of the Code provides that patients have the right to be treated with respect. Failure to disclose risk of harm involves tacit deception – respect for patient autonomy supports a truthful and honest disclosure.
Right to be protected from dishonest coercion and exploitation – medical malpractice fraud Right 2, every consumer has the right to be free to freedom from discrimination, coercion, harassment, and exploitation. Every consumer has the right to be free form coercion by the surgeon forcing them to a single treatment solution, blocking them from alternative treatment options. Right 7, right to make an informed choice Services may be provided to a consumer only if that consumer makes an informed choice and gives informed consent. Without this information, patients are denied the opportunity to legally give informed consent. |
Further evidence, Other consent form extracts:
“ I have had adequate opportunity to ask questions and received all the information I want and I agree to the operation or procedures “
Hawke’s Bay District Health Board
“ I have disucssed with [insert surgeon name here] whose signiture appears on the following page. He/She has explained the reason for and possible risks of the procedure, relating to my clinical history and condtion. I have had an aqequate opportunity to ask questions and have received all the infromation I want. I understand I can ask for more infomration if I wish”
Marlborough District Health Board
“ I have been able to disucss ths with [insert surgeon name here]. He/She has explained the reason for, and expected risks, of the procedure, relating to my clinical history and condtion. and I agree to this treatment / procedures. I have had aqequate opportunity to ask questions and these have been answered to my satisfaction”
Auckland District Health Board
“I have had explained to me the nature of my / the patients condition, the procedure and options for treatment.”
“I have been provide with an assessment of the potential benefits, common side effects and likely outcome of the procedures”
“I have had explained to me situations that may arise during the procedures and complications.
I have had the opportunity to ask questions and I am satisfied with the explanations and answers to these questions.”
Tairawhiti District Health
Appendices
History – Surgeons have always lied about Laparoscopic Cholecystectomy
Some background on the surgeon’s business model: During the late 1980’s operative treatment for gallstones were challenged by alternative treatment. Over the past several decades’ nonsurgical treatment of gallbladder stones were evaluated and gained some popularity, these included the following:
- Oral medical dissolution
- Percutaneous cholecystostomy with stone extraction
- Percutaneous or transnasal topical solvent dissolution
- Extracorporeal shock wave lithotripsy.
This resulted in a marked decrease in surgeries performed because these treatments worked, along with a greater understanding of causes behind Cholecystitis.
One Scottish study showed cholecystectomies decreasing 1% per year, and then laparoscopic cholecystectomies came onto the market for patient services.
This survey determined the effect of the introduction of laparoscopic cholecystectomy on the rates of cholecystectomy (total and laparoscopic) in Scotland. From 1977 to 1990, the Scottish cholecystectomy rate fell by an average of almost 1% per annum. With the advent of laparoscopic cholecystectomy, the total cholecystectomy rate (open and laparoscopic) rose considerably – by 18.7% from 1989-93 (p < 0.05).
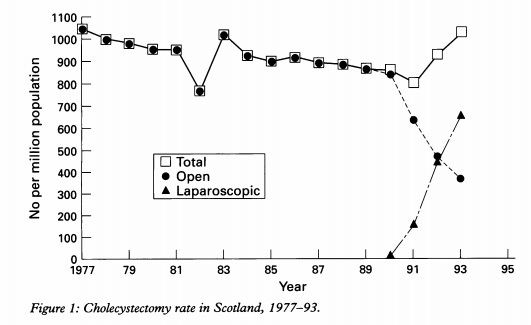
The largest increase (25%) was observed in the 45-64 years age group but it was also particularly evident (19%) in elderly patients (65-74 years). Subjects were more likely to undergo laparoscopic cholecystectomy than open cholecystectomy if they were young and female. The increased cholecystectomy rate observed merits careful scrutiny and health economic evaluation.
The study noted” The total cholecystectomy rates in two states in the USA have increased since the introduction of laparoscopic cholecystectomy, with estimates of the increase varying from 28-60%. The reasons for this apparent worldwide change are not known. The increased cholecystectomy rate may reflect a lowered surgical threshold (over alternative treatment) but other factors may be operative.
In other words – Surgeons are targeting young healthy unsuspecting women for practice and entrepreneurial exploitation
Source: https://www.ncbi.nlm.nih.gov/pubmed/8801212
Surgeons invented a new cash cow income stream to recover from providential loss to alternative treatment options – the laparoscopic cholecystectomy. During the early 1990s adoption, there was a 29% increase in the number of cholecystectomies performed; with over a 100% increase in cholecystectomy for acute acalculous cholecystitis and a 300% increase for biliary dyskinesia.
One US Private practice study revealed cholecystectomies increased 159% following the introduction of laparoscopic cholecystectomy, and went on to say:
“It seems that the use of laparoscopic cholecystectomy, a new technology touted as reducing health care costs, may result in an increased consumption of health care resources due to changes in the indications for gallbladder surgery”. (JAMA. 1993;270:1429-1432″
In other words, the thresholds and criteria for diagnosing surgery were changed to generate income.
http://gut.bmj.com/content/gutjnl/38/2/282.full.pdf
The problems of this new surgery procedure was two-fold:
- Patients were needed for procedural development and training (experimentation); and
- Justifications were needed for the increased diagnosis of gallbladder removals, to lower the threshold for the surgery treatment option.
A story was invented and is still in practice today. The following information is seen on all consent forms:
1] The gallbladder is, in fact, an unnecessary vestigial organ (prehistoric) not needed.
2] Once removed, the patient can return to a normal healthy diet and live a normal life.
3] The gallbladder can be removed with no likely side effect risks or digestive problems, as bile is now delivered directly to the stomach.
The true injury rates have been trivialised and the side effect risks have never been disclosed.
